Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In the world of microbiology, considering the interaction of bacteria and human blood cells can present a truly fascinating area of study. Central to this discourse is a phenomenon known as Haemolysis, which, in simplest terms, refers to the breakdown or destruction of red blood cells.
On a particular note are some unique bacteria – Streptococci – that possess the ability to cause such hemolysis. Their impact on our health can be significant and varies based on their types and the kinds of hemolysis they induce. Stay with me as we journey into this interesting aspect of microbiology.
Contents
To understand the term “Haemolysis in Streptococci,” we need to delve into what hemolysis itself means. Derived from the Greek words ‘haima,’ meaning blood, and ‘lysis’, indicating breakdown or destruction, hemolysis refers to the process where red blood cells (erythrocytes) are broken down, causing the release of hemoglobin into surrounding plasma.
You see, under usual circumstances, our red blood cells have a certain lifespan. Once they’ve served their purpose of transporting oxygen throughout our body, they become worn out and meet their end in our spleen – it’s almost poetic! This natural termination is termed biological or physiological hemolysis, and it is completely normal.
But just like any system out there, things may not always work as planned. At times, these red blood cells are destroyed prematurely due to several reasons – maybe an underlying disease condition or external factors such as toxins or pathogens.
When this happens outside the spleen at a faster rate than usual, we refer to it as pathological hemolysis. And this is where our microscopic perpetrators – Streptococci come into play. But more on that later.
Also Read: Unraveling C.difficile: An Insight into Biochemical Testing
Streptococci are a group of gram-positive bacteria that have been classified into various types based on their behaviors, particularly towards human blood cells.
Some Streptococci are relatively harmless, participating in the natural microbiota balance residing in our bodies like uninvited yet non-disturbing guests. But others? Not so much; they can cause numerous infections and diseases.
Fascinatingly, several types of this bacterium have a remarkable ability – the capacity to undergo hemolysis – to break down human red blood cells prematurely.
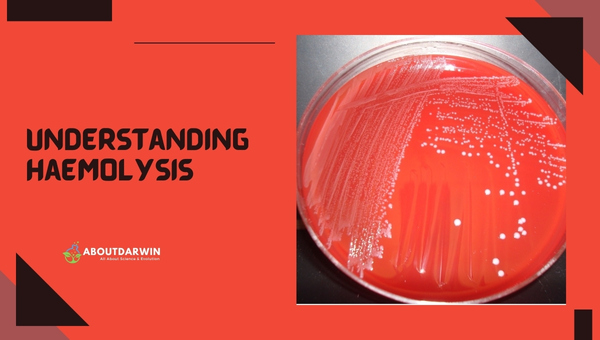
When this particular action happens under lab conditions (such as when we grow these bacteria on blood agar plates), we’re able to witness hemolysis firsthand; it’s almost like watching a microscopic crime scene under a microscope!
The Streptococci pull off this process with the help of enzymes known as hemolysins that get along too well with our erythrocytes (not ideal for us!). Hemolysins attack the red cell membrane, destabilizing it until it bursts open, leading to hemolysis.
This process not only aids in identifying these bacteria but also contributes significantly to their virulence, making some forms of streptococcus notorious disease instigators.
It’s easy to dismiss bacteria and their shenanigans as inconsequential micro-warfare. But let me assure you – the implications of untreated hemolytic Streptococcus infections can permeate into serious health complications that extend beyond mere discomfort.
Alpha Haemolysis happens when certain enzymes produced by the bacteria partially destroy the hemoglobin within red blood cells, creating a greenish discoloration around bacterial colonies on blood agar plates. This action doesn’t result in any full death of the cells but merely causes damage. An example here would be Streptococcus pneumoniae, better known by many for causing ‘pneumonia.’
Beta hemolysis, on the other hand, is where things get messy. It causes the destruction or lysis of red blood cells around a bacterial colony, giving a clear appearance on the agar plate.
In this case, streptococci produce hemolysin enzymes that puncture and disrupt our red cell membranes—leading to cell death. Streptococcus pyogenes falls into this category – always ready to cause conditions like strep throat or scarlet fever.
Also Read: Distinguishing S. pneumoniae and Viridans Streptococci
And then we have Gamma-haemolytic (or non-hemolytic) streptococci – these guys are do-nothings when it comes to breaking down red blood cells—no visible change on blood agar plates surrounds them—a clear case of no harm done!
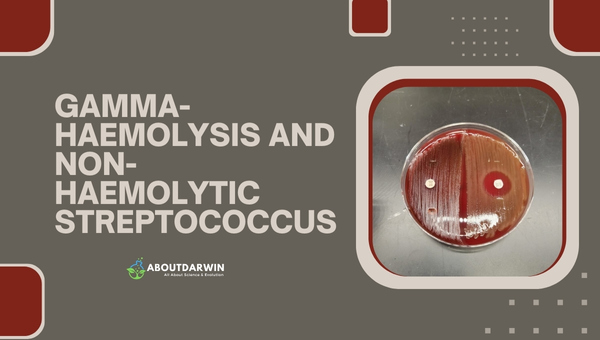
However, that doesn’t mean they can’t cause disease! Take non-hemolytic bacteria like Streptococcus milleri; although shy with hemolysis, they can still pack a punch in causing mild infections under the right circumstances in humans! We must remember not to underestimate these microscopic entities, even if they seem quiet at first glance!
The health implications of untreated hemolytic streptococcus bacteria can be quite severe. In fact, these seemingly tiny microbes can turn our entire world upside down if not appropriately addressed.
We mentioned beta-hemolytic Streptococcus pyogenes earlier, right? If not treated quickly and correctly, you can end up with a nasty case of rheumatic fever—a condition that may cause long-term harm to your heart valves.
Or perhaps you will encounter kidney inflammation (post-streptococcal glomerulonephritis), which arises as your immune system overreacts to the strep infection.
Think alpha-hemolytics like Streptococcus pneumoniae are any kinder? Think again! Unchecked, they can produce life-threatening conditions like pneumonia – a lung infection leading to difficulty in breathing due to accumulation of fluid in the lungs or meningitis- an inflammation of the protective membranes covering the brain and spinal cord.
It pains me to admit it, but these little devils called strep bacteria, when left untreated, hold the power to change lives—and I sadly don’t mean for the better!
Understanding the ways in which these pathogens are transmitted and identifying the key measures for prevention and treatment are crucial in reducing their impact on public health.
With proper hygiene practices and timely medical intervention, the incidence of complications from Hemolytic Streptococcus infections can be significantly diminished.
When it comes to hemolytic Streptococcus infections, early detection is the key to effective treatment. Thankfully, our medical professionals are equipped with several methods to nab these culprits in the act.
The go-to technique is through a culture test – which typically involves swabbing from the throat or other infected sites and growing them on a blood agar plate under specific conditions conducive to strep growth.
The results? Identifiable by different reactions to red blood cells, as we discussed – destruction (Beta hemolysis), partial (Alpha hemolysis), or no harm at all (Gamma hemolysis). These findings can then be attributed to the respective strep species aiding proper diagnosis.
For prevention strategies against hemolytic Streptococcus infections, I always resort back to my favorite maxims: “Cleanliness is next to godliness” and “prevention is better than cure.”
Strict adherence to proper hygiene practices like frequent handwashing, especially if in contact with individuals already infected, ensures you stand guard against unwanted intruders such as these bacteria sneaking into your system.
In cases of recurring infections, administered antibiotics act as prophylactics, halting bacterial proliferation and nipping it in its bud. Vaccination drives like the Pneumococcal vaccine against Streptococcus pneumoniae precisely aid this cause, rendering us a robust army ready for combat!
Also Read: Identifying Shigella Flexneri: A Deep Dive into Biochemical Testing
Beta-hemolysis is complete hemolysis.
Hemolysis is the lysis of red blood cells in the blood due to the extracellular enzymes produced by certain bacterial species.
A chemically defined medium has now been developed for the growth of Streptococcus mutans. The nutritional requirements proved to be simple. Except for the vitamins required, ammonia could serve as the sole source of nitrogen for the growth of the organism.
Hemolysis is the medical term used to describe the destruction of red blood cells.
We’ve journeyed through the world of Streptococcus bacteria and their various types, diving into alpha, beta, and gamma hemolysis. Understanding what these terms mean and how they are linked to specific bacterial types can be mind-boggling initially. Yet it’s paramount to grasp these concepts, thanks to the health implications they have on us.
Early recognition and intervention are vital when dealing with hemolytic strep infections – no matter what type. Respect hygiene rules, keep up a strong defense mechanism via ennobling immunity, and seek medical help at the earliest signs of infection—these actions will always stand you in good stead.